A deeper look at clinicians’ perception of healthcare in rural America
Editor's Note: This blog was published prior to the transition to WebMD Ignite.
New research finds that rural healthcare professionals’ top concern is quality of care.
The health disparities between rural areas and non-rural areas have been well documented, with individuals who live in rural counties reporting worse physical health compared with residents of large non-rural counties. Rural Americans are at greater risk for heart disease, cancer, and stroke than their non-rural counterparts, according to studies from the Centers for Disease Control and Prevention (CDC).
To better understand these disparities and what they mean for care delivery, Medscape, a WebMD company, and Walmart recently surveyed those on the front lines of health care in rural and non-rural communities — primary care physicians, physician assistants, nurse practitioners, registered nurses, pharmacists, and optometrists — and summarized the findings in a report called Healthcare Professionals’ Perspectives on Health Care in Rural America.
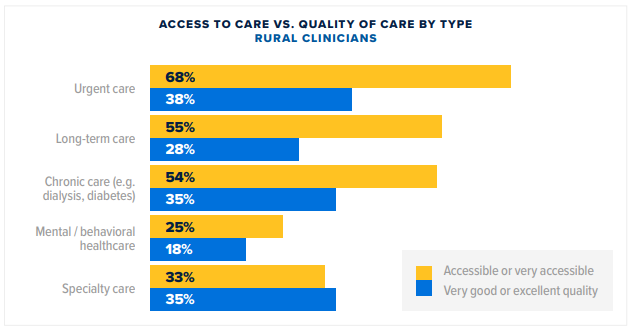
One of the most significant findings was that quality of care was most concerning to primary care providers in rural healthcare professionals – outranking even concerns over access.
For example, less than two-fifths (38%) of rural healthcare professionals rated the quality of specialty, urgent and chronic care as high, compared to more than half of non-rural professionals.
However, the survey also found that technology alone won’t close these gaps, with a significant divide in clinicians’ comfort with and interest in some health technologies, particularly remote patient monitoring and personal health technology. Although the majority of healthcare professionals indicated they were comfortable using telehealth and electronic health records, the findings still show an overall need to help healthcare professionals develop a firm grasp of health technologies’ value and functionality to make better use of the tools.
When asked what general factors would most improve the quality of their care, rural healthcare professionals cited more staff, better community support systems, such as community health programs to help patients outside the doctor’s office, and patient financial assistance.
“These survey findings illustrate that new and innovative approaches are needed to transform the delivery of care,” said Marissa Badders, MSHI, BSN, RN, CPN, senior clinical advisor, at WebMD Provider Services. “Broadening the care model to be more team-based and supplementing the clinician-patient relationship with patient education during their care journey can help close gaps in the quality of rural care.”




